banner by Matthew Stoss and Maureen Borden
Optogenetics: Illuminating the Intricacies of the Human Brain
by Muhammad Feroze
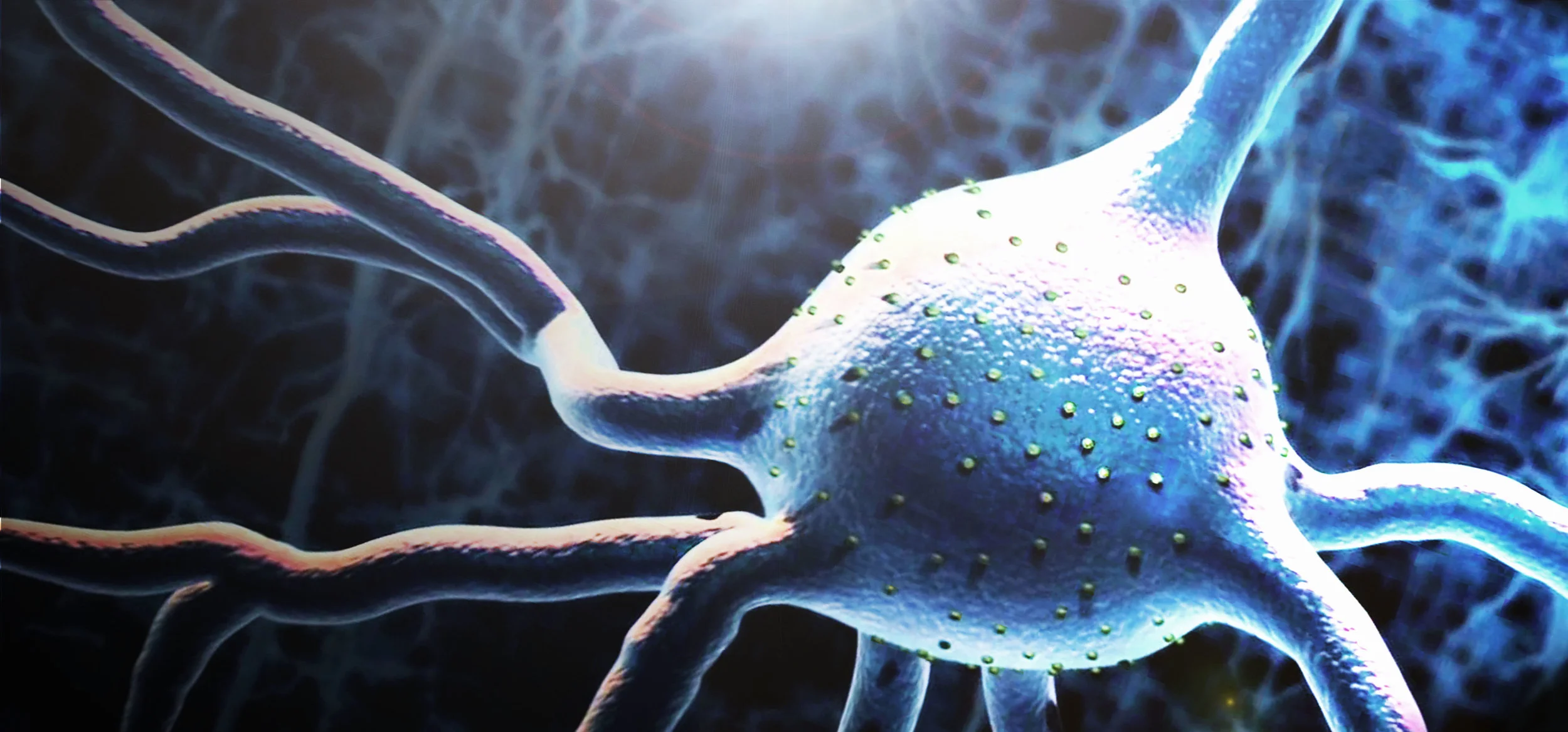
Imagine using light to treat health issues ranging from spinal cord injuries to vision disorders. Devising new therapies with this innovative approach may seem far-fetched, but it has garnered the attention of many neuroscientists and biomedical researchers. By combining optical and genetic techniques, optogenetics enables the selective activation and silencing of neurons, cells that transmit information through electrical and chemical signals in the nervous system.
Neuroscience is a highly interdisciplinary field that combines subjects, such as molecular biology, electrophysiology and computational modeling. Ongoing developments in neuroscience use techniques from each of these fields. Optogenetics is perhaps the most recent example of an interdisciplinary tool and involves the control of neuronal activity with light. The technique shows limitless potential, which has prompted neuroscientists to use it to map neural circuits and for direct clinical applications.
Dr. Karl Deisseroth, a professor of bioengineering and psychiatry at Stanford University and a practicing psychiatrist, helped pioneer the use of light to stimulate neurons in the early 2000s. Motivated by the need to characterize mental illnesses, such as depression and anxiety disorders, Deisseroth and his team of collaborators have harnessed the power of light-sensitive molecules called opsins for insertion into nerve cells. Opsins are molecules found in a variety organisms, such as humans and microbes. In humans, opsins are present in the retina of the eye. However, these opsins must activate additional proteins to transform light into electrical signals used for neurons to communicate.
As cellular membrane proteins, opsins can influence the charge across a cellular membrane, allowing them to regulate electrical activity. The key lies in the light-activated properties of opsins, which allows for the modulation of a neuron’s activity. Adding the opsin into the cell membrane resembles installing a switch to control when ions flow and electrical signals are created. Therefore, exposing the cells to light turns the switch on and off. Incorporating opsins into cells is relatively straightforward. It involves pairing the opsin gene with a benign non-replicating virus. As the virus spreads from the injection site, neurons selectively express the genetic code for the opsin.
Deisseroth and two of his graduate students, Edward Boyden and Feng Zhang, published their first scientific paper on optogenetics in Nature Neuroscience in 2005. In their initial studies, the team used Channelrhodopsin-2, a specific opsin isolated from algae, and integrated it into cultured mammalian neurons. Not only were they able to successfully express the opsins in cells, but they could elicit electrical activity within milliseconds.
A unique aspect of optogenetics is the capacity for the stimulation of neurons in living organisms, rather than solely in a laboratory culture of neurons. This could be revolutionary in medicine as current invasive procedures, such as deep brain stimulation, are relatively crude. However, a system must be implemented to provide light to complement the integrated opsins.
But how can the light be delivered?
A variety of obstacles exists when implanting a light-emitting device into the human body. In addition, for many conditions, it is not yet known which neural circuits should be excited or inhibited to correct the malady. For example, in a spinal cord injury, connections between the spinal cord and the peripheral nervous system are severely damaged, thus limiting muscle function. To address this, researchers are exploring the effects of stimulating motor neurons to restore muscle function.
How does one designate which nerve cells are excited or inhibited? The answer lies in using genetics to direct the expression of opsins to specific pathways in the brain. A key aspect relies on the differential expression of DNA by neurons, which leads to differences in their shape and function. Neurons, like all cells, have enzymes and specific tools to read certain stretches of DNA that regulate gene expression, known as promoter sites. Chemically attaching the right promoter site to the DNA of an opsin will ensure that only certain cells express the foreign protein.
The use of optogenetics to study neurological disorders may engender new avenues to detect and treat malfunctioning circuits. The most salient application of this treatment would involve silencing neurons that contribute to detrimental circuitry and brain dysfunction. This is the approach taken by researchers at Circuit Therapeutics, a biotechnology company from Menlo Park, Calif. Their scientists worked on inhibiting neurons linked to chronic pain in rodents by shining a light on the affected region of skin. They successfully alleviated the pain of a sensitive rodent. The neurons causing this pain are located at the skin, and were easy to access access. Chris Towne, the director of Gene Therapy at Circuit Therapeutics, proposes using a light-emitting patch for patients with high pain sensitivity. This group intends to begin clinical trials for targeting chronic pain soon.
One of the many potential clinical uses for optogenetics regards treating mental illnesses. Every day, psychiatrists at the UPMC Western Psychiatric Institute diagnose and treat dozens of patients with mental illnesses, often resorting to an array of antidepressants. However, the underlying causes of these diseases remain obscure, and these doctors desire a comprehensive understanding of these disorders along with more efficacious treatments. An expanded knowledge of mental illnesses will also aid in eliminating stigmatization. Until recently, this limited understanding of what contributes to mental illness has been fueled by the limitations for intervention at the cellular level. Throughout the last century, researchers lacked such a technique to influence neuronal activity, although opsins were studied decades before the foundation of optogenetics.
Unfortunately, choosing which neurons to target for mental illnesses is not as straightforward as it is for other disorders. The imbalances in neurons and abnormalities in signaling that characterize psychiatric disease must be defined more concretely. Still, researchers have made significant progress using optogenetics. For example, in a recent paper, “Optogenetics and the Circuit Dynamics of Psychiatric Disease,” Deisseroth describes how optogenetics has allowed for identification of the role of certain pathways to control anxiety, depression and addiction.
While the role of optogenetics as a therapy remains nascent, it has shown promise. It is conceivable that doctors will use optogenetics directly as a therapy in many ways in the future, making it a groundbreaking advancement for biomedical researchers who now have unprecedented control over the nervous system.