Banner by Khusbu Patel
Phage Fever
By Maya Albanowski
You wake up with a sore throat, your mom takes you to the pediatrician, the doctor does a throat swab that makes you gag, you go home with a prescription for penicillin (or if you’re allergic like me, amoxicillin). For years, the world took for granted the scientific miracle contained in that pink goo of antibiotics, but for the next generation of little kids with sore throats, those same medications might not work.
The Centers for Disease Control and Prevention names antibiotic resistance (AR) as “one of the world’s most urgent public health problems.” Among the antibiotic resistant pathogens posing the most risk to global public health according to the CDC’s 2019 AR Threats Report, you’ll see some familiar names that’d make any health care provider shudder, such as Clostridioides difficile (C. diff), a bacteria responsible for causing life-threatening diarrhea. Also on this list of dangerous superbugs are Methicillin-resistant Staphylococcus aureus (MRSA), a staph infection commonly spread in hospitals, and Mycobacterium tuberculosis (tuberculosis), a respiratory illness which frequently causes death worldwide. However, there are many pathogens on the list that are not typically thought of as deadly, such as Neisseria gonorrhoeae. To most college students, gonorrhea is a horror story told to them by their high school health teacher and is not typically thought of as causing a difficult to treat infection that could cause life-threatening complications such as ectopic pregnancy.
This rapidly approaching crisis has led scientists on an exigent research endeavor: finding an effective substitute for antibiotics and finding one fast. There are many proposed solutions still being researched, including antimicrobial peptides, CRISPR/Cas9 genetic engineering, probiotics, antibodies and even tiny viruses called bacteriophages.
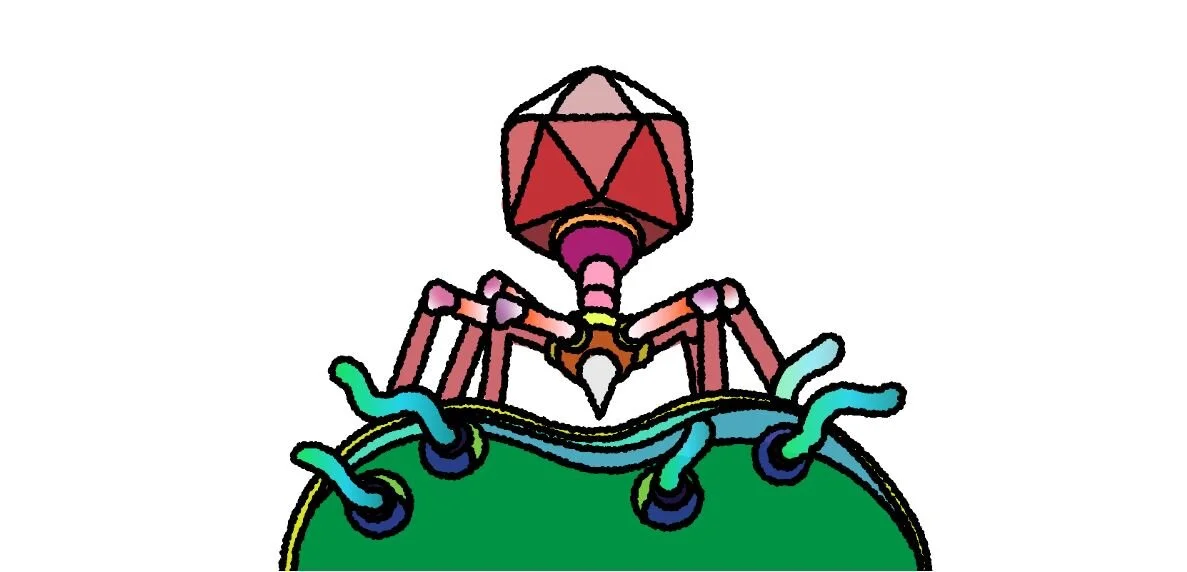
Bacteriophages, or “phages” as they are commonly known, are different than the viruses that give you a stuffy nose and a sore throat, because they only attack bacteria. In the early 20th century, phages were used by researchers to treat cholera and other deadly infections. Phage research was quickly made irrelevant by the discovery of antibiotics, and research into phages’ therapeutic uses was virtually abandoned for decades until the dawn of antibiotic resistance. These bacteriophages are specific to the type of bacteria they kill, so they will not kill beneficial bacteria in the body. Because of this, it takes a long time to develop the right cocktail of phages to effectively treat a patient — a process made simpler by having a database with a large number of known phages at a researcher’s fingertips.
This is where the SEA-PHAGES program comes into play. SEA-PHAGES stands for Science Education Alliance-Phage Hunters Advancing Genomics and Evolutionary Science and is a course available at more than 100 universities internationally. The program is spearheaded by the Hatfull Lab at the University of Pittsburgh and Pitt has one of the largest student populations in the program. The SEA-PHAGES program teaches undergraduates about phage biology by helping them discover their own bacteriophages and characterize them through wet bench lab techniques and bioinformatics. Phages discovered from the SEA-PHAGES program can later be used by researchers to develop a variety of genetic and clinical tools. At Pitt, this research happens in the very same building in which some of these phages are discovered.
I am currently enrolled in the SEA-PHAGES program and got the opportunity to discover a bacteriophage last semester — I named it Azula and it is a temperate phage from cluster CV. This means that Azula does not kill all of the bacteria that it infects, but instead inserts its genome into the bacterial genome, making these specific phages useful for engineering phages that will kill pathogenic bacteria. Azula is currently in the process of having its genome sequenced by Pitt students who will determine what specific genes are hidden in its base pair sequence.
Dr. Graham Hatfull has been working with phages at the University of Pittsburgh since 1988, but for most of that time, phage therapy has not been an interest. Hatfull considers himself to be “healthily skeptical” of phage therapy but finds phages interesting for a variety of other reasons. His lab mainly works with mycobacteriophages with a purpose of learning more about phages and developing genetic tools for use in biological research. However, in 2017, Dr. Hatfull was contacted by a colleague in London for help treating an antibiotic resistant infection in a 15-year-old cystic fibrosis patient. With a cocktail of three phages all discovered by students from SEA-PHAGES-like programs, the Hatfull lab was able to successfully treat the patient’s Mycobacterium abscessus infection and save her life.
Since that first patient, the Hatfull lab has successfully developed cocktails of phages to treat bacterial infections all over the world, having been able to help treat patients in the United States, United Kingdom and Italy, with plans to expand into Mexico, Spain, Australia and France. According to Hatfull, there are two distinct stages of the process of developing phage therapy, and the process overall can take anywhere from six months to 10 days. The first stage utilizes microbiology techniques to isolate several phages that will kill the bacterial strain and properly preparing them for use in a patient. The second stage involves getting permission from the proper regulatory bodies within the country’s government and health system. Hatfull believes that this part of the process will get easier over time as these agencies become more familiar with phage therapy.
When asked how SEA-PHAGES affects the Hatfull lab’s research, Dr. Hatfull describes the program’s contribution as something they would be “lost without.” While phage therapy is a long way from selling a bottle of phages on a pharmacy shelf, prospects are good with bacterial strains such as Mycobacterium tuberculosis and Pseudomonas. When it comes to finding useful phages to work with in the lab, having 17,000 phages available at your fingertips is an invaluable resource — a resource that essentially puts the development of phage therapy “into fast forward.” These student-discovered phages, like Azula, are a part of a much larger research effort that is building the future of health care right on Pitt’s campus. Undergraduates are saving lives right on Fifth Avenue, and they don’t even have to be doctors or researchers to do it.